
Patients report that reading their notes makes them more likely to take medications as prescribed
BOSTON – A new study of patients reading the visit notes their clinicians write, report positive effects on their use of prescription medications. The study, Patients Managing Medications and Reading their Visit Notes: A survey of OpenNotes participants, published today in the Annals of Internal Medicine, shows that when patients read their notes, they report significant benefits, including feeling more comfortable with and in control of their medications, a greater understanding of medication’s side effects, and being more likely to take medications as prescribed.
The study of approximately 20,000 adult patients at Beth Israel Deaconess Medical Center in Boston (BIDMC) in Boston, at the University of Washington Medicine (UW) in Seattle, and at Geisinger, a health system in rural Pennsylvania was conducted online between June and October of 2017. The three health systems have been sharing visit notes written by primary care doctors, medical and surgical specialists, and other clinicians for several years.
“Sharing clinical notes with patients is a relatively low-cost, low-touch intervention,” said study lead Catherine DesRoches, DrPH, Executive Director of OpenNotes, in the Division of General Medicine at BIDMC and an Associate Professor of Medicine at Harvard Medical School. “While note sharing requires a culture shift in medicine, it is not technically difficult with most Electronic Health Record Systems (EHRs), and could have an enormous payoff, given that we know poor adherence to medications costs the health care system about $300 billion per year. Anything that we can do to improve adherence to medications has significant value.”
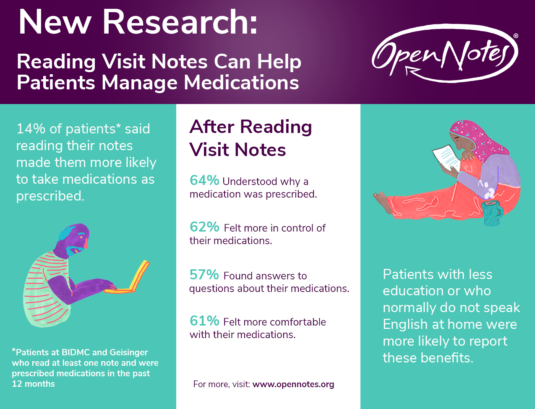
Patients reported that they gained important benefits from reading their notes: 64 percent reported increased understanding of why a medication was prescribed; 62 percent felt more in control of their medications; 57 percent found answers to questions about medications; and 61 percent felt more comfortable with medications. Fourteen percent of patients at BIDMC and Geisinger said that they were more likely to take their medications as prescribed after reading their notes, while 33% of patients at UW rated notes as very important in helping them with their medications. The study also showed that patients speaking primary languages other than English and those with lower levels of formal education were more likely to report benefits.
“This kind of transparent communication presents a big change in long-standing practice, and it’s not easy,” said study co-author and OpenNotes co-founder Tom Delbanco, MD, MACP, John F. Keane & Family Professor of Medicine at Harvard Medical School and BIDMC. “Doctors contemplating it for the first time are nervous. They worry about many things, including potential effects on their workflow, and scaring their patients. But once they start, we know of few doctors who decide to stop, and patients overwhelmingly love it. The promise it holds for medication adherence is enormous, and we are really excited by these findings.”
Study participants were aged 18 years or older, had logged into the secure patient portal at least once in the previous 12 months, had at least one ambulatory visit note available and had been prescribed or were taking medications in the previous 12 months. The survey respondents represented urban and rural settings, varied levels of education, and broad age and racial distributions. The main outcome measures included patient-reported behaviors and their perceptions concerning benefits versus risks.
In an accompanying editorial, David Blumenthal, MD and Melinda K. Abrams, MS of the Commonwealth Fund write: “Transparency is no longer the distant, radical vision it was when the pioneering OpenNotes team began their work. Rather, it is a fact of clinical life, mandated by federal law and policy…Our challenge now is to make the best and most of shared health care information as a tool for clinical management and health improvement.”
In addition to DesRoches and Delbanco, co-authors include Sigall Bell, MD, Zhiyong Dong, MS, Leonor Fernandez, MD, Patricia Fitzgerald, MSc, and Jan Walker RN, MBA of BIDMC; Joann Elmore, MD of the David Geffen School of Medicine at the University of California Los Angeles (UCLA); and Joshua M. Liao, MD, MSc, and Thomas Payne, MD, FACMI of University of Washington (UW) Medical School.
This work was supported by the Robert Wood Johnson Foundation, Gordon and Betty Moore Foundation, Peterson Center on Healthcare, and the Cambia Health Foundation. The funders had no role in designing or conducting the study, analyzing the data, preparing the manuscript, or deciding to submit this manuscript for publication.
The authors declare no competing interests.
About OpenNotes
OpenNotes is an international movement that urges doctors, nurses, therapists, and others to invite patients to read the notes they write to describe a visit. These shared clinical notes, known increasingly as “open notes,” are spreading throughout the U.S. OpenNotes is based at Beth Israel Deaconess Medical Center in Boston. To learn more, visit www.opennotes.org.
About Beth Israel Deaconess Medical Center
Beth Israel Deaconess Medical Center is a patient care, teaching and research affiliate of Harvard Medical School and consistently ranks as a national leader among independent hospitals in National Institutes of Health funding.
BIDMC is in the community with Beth Israel Deaconess Hospital-Milton, Beth Israel Deaconess Hospital-Needham, Beth Israel Deaconess Hospital-Plymouth, Anna Jaques Hospital, Cambridge Health Alliance, Lawrence General Hospital, Signature Healthcare, Beth Israel Deaconess HealthCare, Community Care Alliance and Atrius Health. BIDMC is also clinically affiliated with the Joslin Diabetes Center and Hebrew Rehabilitation Center and is a research partner of Dana-Farber/Harvard Cancer Center and the Jackson Laboratory. BIDMC is the official hospital of the Boston Red Sox. For more information, visit www.bidmc.org.




You must be logged in to post a comment.