This piece offers practical guidelines for documenting IPV in trauma-informed, patient-centered ways, while navigating transparency requirements under the Cures Act. It acknowledges proxy access features and risks, but focuses on how OpenNotes can be used safely to empower survivors and build trust.
Implementation
Solutions for Increased Adoption of Patient Portal Shared Access: A Human-Centered Design Approach Using the Double Diamond Model
Using a human-centered design approach, OpenNotes and researchers at the Johns Hopkins Bloomberg School of Public Health explored how to improve awareness and adoption of shared access to patient portals for older adults and their care partners.
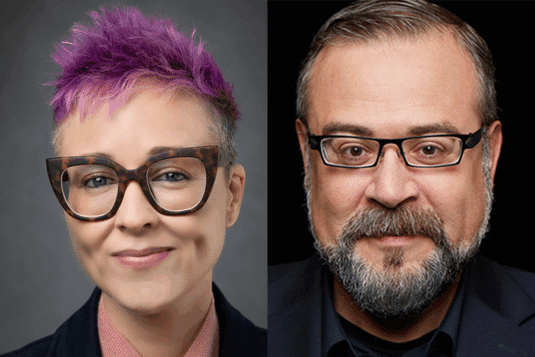
Critical AI Health Literacy as Liberation Technology: A New Skill for Patient Empowerment
As artificial intelligence transforms health care, patients are increasingly using generative AI to question, reinterpret, and even resist institutional decisions. This provocative commentary, from Hugo Campos and Liz Salmi, introduces “Critical AI Health Literacy” as a new skill set for patients seeking agency and equity in the digital age of medicine.
Identifying, engaging, and supporting care partners in primary care settings: a portal-based intervention
Millions of Americans are care partners but they are rarely identified or supported in care delivery. With a portal-based questionnaire, we identified participants with caregiving responsibilities and further evaluated them in order to offer support.
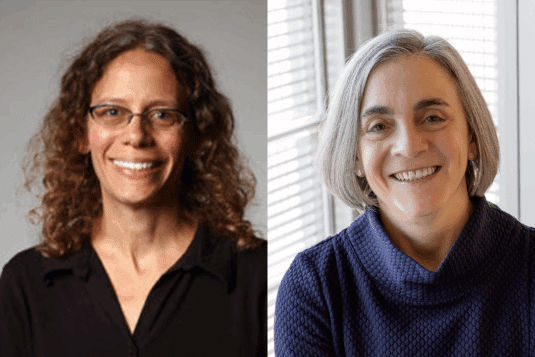
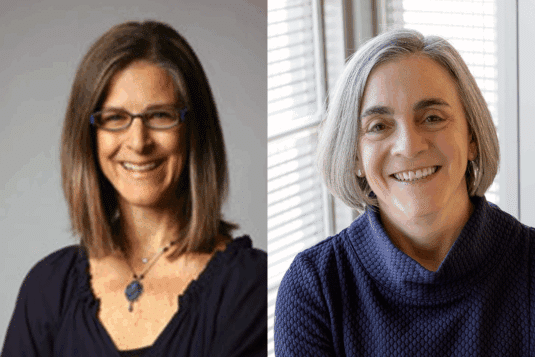
Whom Should We Regard as a Legitimate Stakeholder in the Accuracy of Information in a Patient’s EHR?
This case describes a care partner who was distressed by bias and inaccuracies in a loved one’s medical notes. Steve O’Neill LICSW, BCD, JD and Catherine M. DesRoches, DrPH, MSc offer guidance on how the doctors and hospital should respond.
Which Patients With Cancer Access Their Clinical Notes? A Disparities Analysis
Although clinician notes are now available to all patients, many of the most vulnerable populations are less likely to read them. This study tracks how ethnicity, race, and language impact who is opening their notes at a high-volume specialty cancer center.
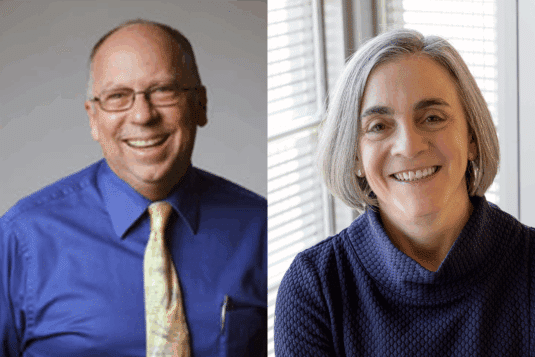
Near-wins in the pursuit of quality: does transparency matter if no one is looking?
In this new editorial for BMJ Quality & Safety, Sigall Bell, MD and Cait DesRoches, DrPH reflect on how access to medical notes can improve the quality of care, but only if patients are able to read and understand them. In the time between medical visits, when patients are monitoring their own health, AI may open a new frontier.
Changes in Documentation After Implementing Open Notes in Mental Health Care: Pre-Post Mixed Methods Study
https://doi.org/10.2196/72667 Background The practice of providing patients with digital access to clinical narrative documentation by health care professionals (HCPs) is known as open notes. In mental health care, this innovation has the potential to increase transparency and foster greater trust in the treatment process. While open notes may improve the quality of care and patient…
Chaplains’ Charting in the USA in the Era of “Open Notes:” Recommendations from a Quality Improvement Project
This paper addressed the particular needs of chaplains in oncology settings where relationships tend to be longer. It recommends using strengths-based language, avoiding language that suggests disbelief, shortening notes, and using documentation to extend spiritual care.
A multicenter randomized trial to improve family clinical note access and outcomes for hospitalized children: The Bedside Notes study protocol
https://doi.org/10.1002/jhm.70155 Introduction The 2021 Cures Act mandates caregiver access to their child′s medical notes with few exceptions, yet fewer than 10% access notes during hospitalization. Caregiver review of real-time notes facilitates identification of safety concerns and may enhance patient safety in pediatric hospitals. This trial will evaluate the Bedside Notes intervention—a multifaceted approach to enhance…